A Delta Variant Q&A with Dr. David A. Wein
Tuesday, August 10, 2021
David A. Wein, M.D. is the Chief of Emergency Medicine at Tampa General Hospital, System Medical Director for TeamHealth, and an Associate Professor at USF Morsani College of Medicine.
This past March, we published what we hoped would be our final Q&A with Dr. David A. Wein on the Covid-19 pandemic. Our optimism grew even stronger in April and May as the vaccination campaign brought the numbers down in near-miraculous fashion. Unfortunately, the delta variant has changed all that. Over the past three weeks, several readers, family members and friends asked us for another update, and a few posed some specific questions. Here are some highlights from the resulting conversation.
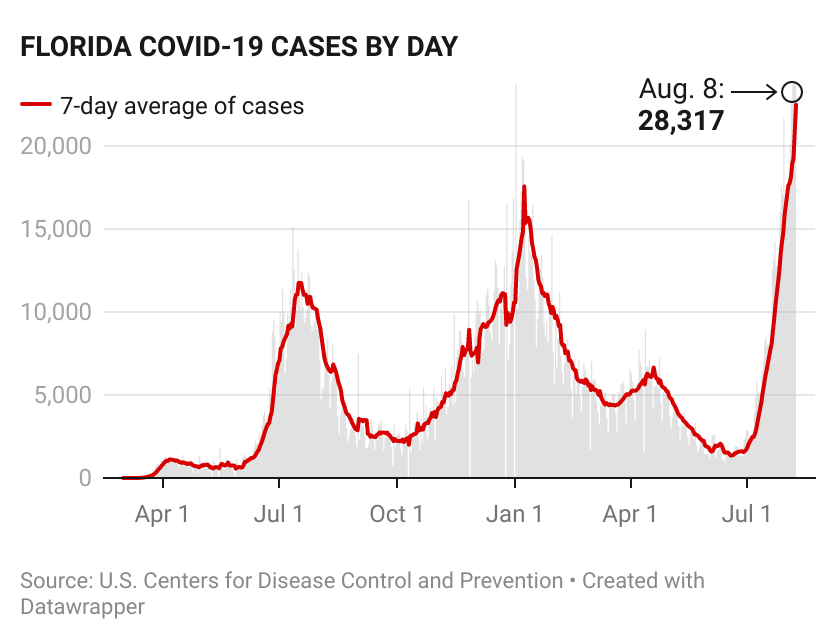
Rachel Elias Wein: It feels like we’re the epicenter of this fourth wave. The CDC just reported that Florida had 23,903 cases on August 7—the state’s highest single-day total since the pandemic started. As we speak, there are more than 13,793 Covid patients in Florida hospitals. Can you tell us what you’re seeing in the emergency department at Tampa General?
Dr. David A. Wein: Unfortunately, Florida and Louisiana are the country’s two hottest spots at the moment, with largely a delta variant outbreak similar to what we saw in Missouri earlier in the summer. For us at Tampa General, the total number of cases that we’re seeing, in terms of hospitalizations and acuity, is very much like what we saw during our winter peak. We had more than 100 hospitalized patients back then and are significantly above that today.
REW: And what are you seeing with respect to breakthrough cases?
DAW: We’re seeing exactly what medical professionals have reported elsewhere in the country: Most Covid-19 patients who need to be hospitalized—almost all of them—are unvaccinated. Right now, almost all of those who end up in the hospital needing critical care are unvaccinated.
REW: And what about the hospitalization of those with breakthrough infections?
DAW: Typically, those are patients who have poorly functioning immune systems from other serious medical conditions. Maybe they had an organ transplant, for example, and their immune system just has not mounted an appropriate response to receiving the vaccine. It is almost as though these patients were never vaccinated.
Outside of hospitalization, we have close friends who are fully vaccinated and yet became infected. Several of our fully vaccinated doctors and other healthcare workers have had breakthrough infections.
They get sick for a bit—cold and flu types of symptoms—but generally haven’t had to be hospitalized. That’s the important thing. They are not at any risk of a life-threatening disease.
REW: It’s clear to me that many people aren’t exactly sure how they should respond to what’s happening. Probably the question I get asked most frequently is how we, as a family, have changed our behavior. How would you characterize that?
DAW: If you go back a few weeks or months, most of our behaviors had largely returned to normal. We had reached a point where I felt comfortable going into indoor spaces without a mask, even if we were going to be there for a long time. We were just going about our normal daily routines.
It’s important to note that individual situations matter a lot here. We have younger children who are not able to be vaccinated yet. That has led us to take extra care with anything they do. So they have worn masks indoors from the beginning of the pandemic. And now, anywhere we go with them, we’re wearing masks, too.
We’re rarely eating at restaurants now. And if we do, we’re outdoors. And because we have unvaccinated children, we’re not flying anywhere with them.
REW: Another decision we made was to move all three children to schools that require 100 percent masking indoors. We did that last year.
DAW: Yes. We’re doing everything we can to maintain a sense of normalcy—certainly, we’re taking advantage of outdoor recreational activities, where there’s quite a bit of safety—but we’re also being prudent about protecting ourselves and others.
Your readers may want to check out the CDC’s updated current guidelines for the vaccinated. The agency urges vaccinated Americans to wear masks in public indoor settings in areas of ‘substantial’ or ‘high’ transmission. If you look at an online map of those areas, you’ll see that this is basically the entire country at this point.
REW: People have also asked about whether there are any specific treatments if they contract Covid.
DAW: If you have symptoms and test positive, then within 7 to 10 days you could certainly seek monoclonal antibody therapy. It’s an infusion of premade antibodies that fight the virus. They don’t last as long as what you’d get from vaccination, but this treatment can reduce your chances of ending up hospitalized. The treatment is open for adults both vaccinated and unvaccinated. You’d need a physician referral, and the treatment occurs in a medical setting. I would recommend looking in your local area for facilities that offer it.
REW: Another question that came up is about whether you need to get the vaccine if you have had Covid.
DAW: You should definitely get the vaccine. You may want to wait a bit and make sure you are recovered but vaccination is a huge jump in terms of the degree of protection.
REW: Other ‘early adopters’ who were enthusiastic about vaccination are now coming up on six months since their last shot. They wonder when they can get a booster. What are your thoughts on that?
DAW: The FDA will need to approve boosters for the general population and we have no word on that as yet. Reportedly, the agency will make an announcement soon on boosters for the immunocompromised. We’ll see.
Arguably, though, the bigger question is whether wealthier countries like the United States, many of which have an overabundance of vaccines, should be giving boosters, as opposed to aggressively trying to vaccinate people in other, less fortunate countries. This is not just altruism: The reason we have a delta variant is because there was rampant spread in India six or eight months ago. The more a virus replicates, the more it has an opportunity to mutate.
REW: So the more cases there are, the more chances there are that you’re going to get another variant.
DAW: Right, and if we keep having hotspots around the world where there is no control or other measures, eventually we’re going to run into a variant that is even more difficult to control with vaccines, and possibly one that leads to more severe health outcomes.
In addition to the substantial moral and ethical dimension here, it’s so important to get these vaccines to other parts of the world. Protecting as many people as possible is ultimately how we will get this pandemic under control.
REW: When do you think your emergency department will get back to some semblance of normal?
DAW: The projected peak in our area is early September. Given how steeply cases continue to rise, it will probably be a few weeks after that before we start to see the curve get back to something more normal. This past weekend mass testing sites were reopened in Tampa and they closed early due to high demand both days. We are taking steps to further increase our emergency department capacity in the coming days as well to handle the demand.
REW: And what would slow the spread?
DAW: Increasing rates of vaccination, changes in behavior and—unfortunately—more people having already contracted the virus. We will continue to see rolling outbreaks until the pandemic is under control but we have seen peaks and then declines in delta hotspots like Missouri, the United Kingdom and India. It’s expected that something like that will happen here as well.
REW: Is there anything else people should do?
DAW: I definitely recommend getting your flu shot. We’re already seeing a rise in pediatric RSV cases—another respiratory virus—and we could see a resumption of a more normal, or possibly even a worse-than-normal, cold and flu season this year.
REW: This Q&A truly was ‘back by popular demand.’ Hopefully, it will be the final installment of our series.